Alberto Cabrera-Zubizarreta, Antonio Jimenez-Marin, Daniela Ramos-Usuga, Itziar Benito-Sanchez, Endika Martinez-Gutierrez, Victoria Boado, Fermin Labayen, Juan Carlos Arango-Lasprilla, and Jesus M. Cortes. Long-COVID: Aberrant connectivity of salience network in critically-ill patients. OHBM 2022 – Organization for Human Brain Mapping [pdf]
Introduction:
Long-COVID, a.k.a. post COVID syndrome, is a poorly defined systemic con-dition that encompasses fatigue, headaches and muscle aches, memory loss, sleep disorders, concentration problems and attention deficit, among other symptoms. The term “Long-COVID” describes the presence of symp-toms weeks or months after acquiring SARS-COV-2 infection irrespective of the viral status. It can be continuous or relapsing and even new symptoms might appear over time. During long-COVID most of the patients have nega-tive PCR as well as no biochemical or radiological abnormalities, so in this sense long-COVID encompasses a transitory condition from microbiological recovery to clinical recovery. The aim of the study was to explore functional whole-brain dysfunctionality, by assessing resting state networks connectivi-ty of a well-controlled group of critically ill COVID-19 patients.
Methods:
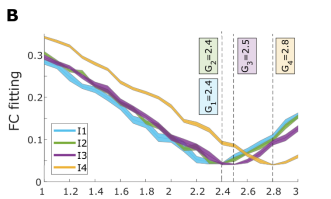
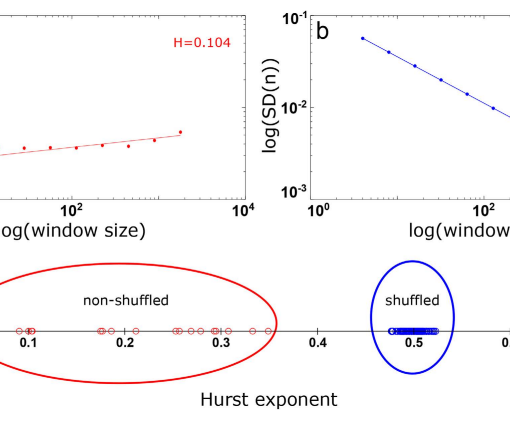
We focused on brain connectivity alterations of the different resting state networks in a cohort of N=15 critically-ill COVID-19 patients as compared to N=15 healthy controls, matched by age and sex. Inclusion criteria were: SARS COV-2 disease confirmed by PCR, age between 18 and 65 years, admission in Intensive Care Unit (ICU), SOFA (Sequential Organ failure Assessment) score equal or bigger than 4, meaning they were severely ill with multi organ failure, Neuro-psychiatric symptoms lasting more than 24 weeks and a normal brain appearance on T1 weighted sequences. Imaging acquisitions were performed six months after Intensive Care Unit (ICU) discharge. Following a similar methodology as in (Jimenez-Marin et al, Neuroimage clinical, 2021), we built functional connectivity matrices at the voxel level (total number 50,125 voxels, 3×3×3mm3 ). Using masks of known resting state networks (RSN) (Yeo et al., J Neurophysiol., 2011), we obtained for each RSN and participant a 3D brain map of strength by summing across all FC values from any voxel in the brain towards all voxels within each RSN.
Results:
Six males and 9 females with a mean age of 56.2 years were included in the study. Mean stay in ICU was 26.85 days and mean SOFA score was 6.15. Mean days from admission to MRI was 218.08. Patients showed neurologi-cal impairment and cognitive assessment revealed differences with controls in learning and memory, Hopkins Verbal Learning Test, (HVLT-R Recall test p 0.01), speed processing and attention, Brief Test of Attention (BTA p=0.03) and Symbol Digit Modalities Test (SDMT p= 0.01), language, verbal fluency test (p < 0.001), but not in executive functioning. Significant differences in salience connectivity were found after multiple-comparisons and for the con-trast patient > control, indicating hyper-connectivity of the salience network (SN) in COVID-19 patients as compared to controls at six months after ICU. Hyper-connectivity occurred from the salience towards visual (39%), soma-tomotor (34%), dorsal attention (30%), ventral attention (18%), limbic (16%), executive frontoparietal (13%) and default mode networks (15%). SN has been implicated in the integration of emotional and sensory stimuli as well as in modulating the switch between the internally directed cognition of the default mode network (DMN) and the externally directed cognition of the central executive network (CEN). SN hyper connectivity has been described in anxiety disorders, post traumatic stress disorder, autism spectrum disorder and schizophrenia and may account for the neuropsychiatric symptoms in long-COVID patients.
Conclusions:
Critically ill COVID-19 patients show resting state network dysfunction with hyper connectivity of the Salience network more than 6 months after the in-fection. For how long these alterations persist in long-COVID remains to be elucidated.