D Ramos-Usuga, A Jimenez-Marin, A Cabrera Zubizarreta, I Benito-Sanchez, D Rivera, E Martinez-Gutierrez, E Panera, V Boado, Fermin Labayen, J M Cortes, Juan C. Arango-Lasprilla. Cognitive and brain connectivity trajectories at one-year post intensive care unit discharge in individuals with COVID-19. Neurorehabilitation. In press, 2024. [pdf]
Abstract
BACKGROUND: Multiple Organ failure (MOF) is one of the main causes of admission to the Intensive Care Unit (ICU) of
patients infected with COVID-19 and can cause short- and long-term neurological deficits.
OBJECTIVE: To compare the cognitive functioning and functional brain connectivity at 6–12 months after discharge in
two groups of individuals with MOF, one due to COVID-19 and the other due to another cause (MOF-group), with a group
of Healthy Controls (HC).
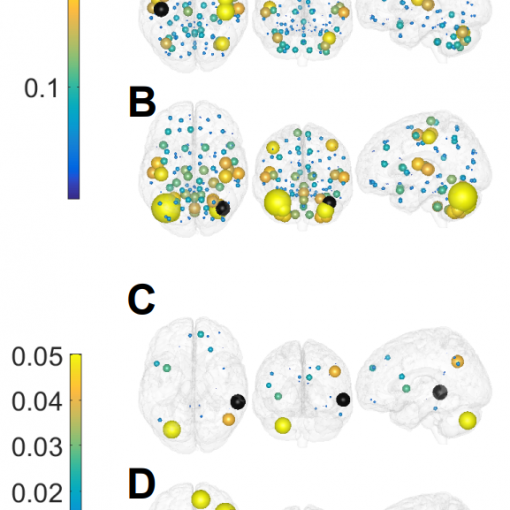
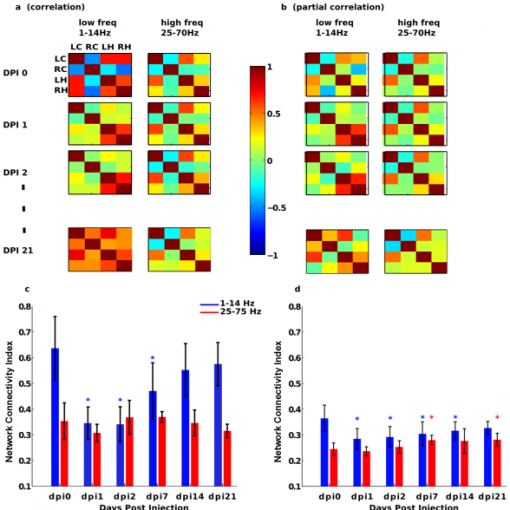
METHODS: Thirty-six participants, 12 from each group, underwent a neuropsychological and neuroimaging assessment
at both time-points. Functional connectivity of the resting state networks was compared between COVID-19 and HC while
controlling for the effect of MOF. The association between functional connectivity and neuropsychological performance was
also investigated.
RESULTS: Compared to the HC, COVID-19 group demonstrated hypoconnectivity between the Default Mode Network
and Salience Network. This pattern was associated with worse performance on tests of attention and information processing
speed, at both time-points.
CONCLUSION: The study of the association between cognitive function and brain functional connectivity in COVID-19
allows the understanding of the short- and long-term neurological alterations of this disease and promotes the development
of intervention programs to improve the quality of life for this understudied population.